Exaggerated response of the tooth to hot, cold or stream of air can be described as dentin hypersensitivity of the tooth. The exogenous stimuli may include thermal, tactile or osmotic changes. While extreme stimuli can make all the teeth hurt, the term hypersensitivity means painful response to stimuli not normally associated with pain.
Dentin hypersensitivity is defined as “sharp, short pain arising from exposed dentin in response to stimuli typically thermal, chemical, tactile or osmotic and which cannot be ascribed to any other form of dental defect or pathology”
The dental pulp is richly innervated with nerves and blood vessels. The nerve group present are the A delta fibres and C fibres majorly. The sharp, better localized pain is mediated by A delta fibers, C fiber activation is connected with the dull radiating pain sensation. Myelinated A fiber are responsible for dentin sensitivity. Tooth hypersensitivity differs from dentinal or pulpal pain. In case of dentin hypersensitivity, patient’s ability to locate the source of pain is very good, whereas in case of pulpal pain, it is very poor
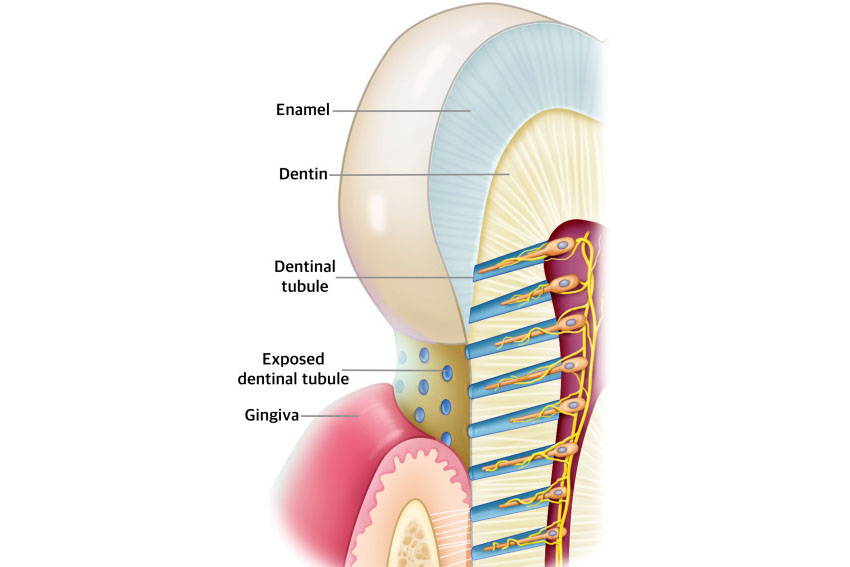
The most accepted theory is the Brannstorm’s hydrodynamic theory which says that displacement of the dentinal tubule contents is rapid enough to deform nerve fiber in pulp or predentin or damage odontoblast cell. This rapid fluid movement activates the mechanoreceptor nerves of A group in the pulp and cause dentinal hypersensitivity.
The primary underlying cause for dentin hypersensitivity is exposed dentinal tubules which can occur either by loss of covering periodontal structures (gingival recession), or by loss of enamel.
Common reasons for gingival recession
Reasons for continued dentinal tubular exposure
Causes of loss of enamel
Home care with dentifrices
In office treatment procedure
Treatments that partially obturate dentinal tubules
Tubule sealant
Miscellaneous
Article by Dr. Siri P.B.

Hailey - 10 months ago